Polypharmacy—the use of five or more medications—is highly prevalent among adults with cancer and multimorbidity, and is associated with high health service utilization, Canadian researchers have found. This was also true of younger adults, and most prevalent among individuals with lung cancer and those diagnosed with stage IV cancers.
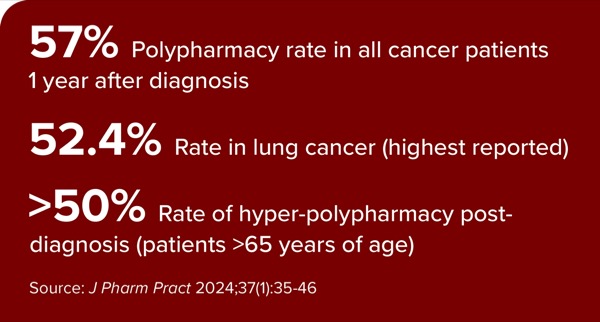
The prevalence of polypharmacy overall was 46% before and 57% one year after diagnosis, according to researchers at Lakehead University, in Thunder Bay, Ontario (J Pharm Pract 2024;37[1]:35-46). During this longitudinal study of 193,047 Ontarians, polypharmacy before and after cancer diagnosis increased with the level of multimorbidity and increasing age but not by sex. It was highest in people with lung cancer (52.4%) and those diagnosed with stage IV cancer (51.3%).
Minor polypharmacy (the use of five to nine drugs) increased the odds of being a high user of the emergency department (ED; 1.16; 99% CI, 1.09-1.24) and more frequently hospitalized (1.03; 99% CI, 0.98-1.09). The odds of high use were greater with hyper-polypharmacy (the use of =10 drugs): 1.41; 99% CI, 1.33-1.51 for ER visits and 1.23; 99% CI, 1.17-1.29 for hospitalizations.
The investigators reviewed de-identified records from health administrative databases of adult Ontario Health Insurance Plan members diagnosed with cancer between April 2010 and March 2013. Polypharmacy was categorized into three groups: less than five drugs (no polypharmacy), minor polypharmacy and hyper-polypharmacy.
They also reviewed ED visits and hospitalizations in the year following cancer diagnoses to determine high usage (being at or above the 90th percentile), and conducted statistical analyses to determine how polypharmacy pre- and post-cancer diagnosis differed by age, sex, multimorbidity, or cancer type or stage.
The mean age of participants was 65.8 years. Overall, breast, lung and bronchus as well as prostate cancers were most prevalent. Cancer stage was unknown for more than half of the study population. About half of the study population had three or more chronic conditions.
The prevalence of minor polypharmacy and hyper-polypharmacy before cancer diagnosis was 20.9% and 25.1%, respectively. While polypharmacy increased after cancer diagnosis, the prevalence of hyper-polypharmacy greatly increased (to 37.8%). The prevalence of hyper-polypharmacy was consistently highest among those 65 years of age and older (about 40% before diagnosis and >50% post-diagnosis), and it more than tripled in younger age groups after diagnosis.
Researchers also found:
- The prevalence of polypharmacy post-cancer diagnosis was five times higher among those without any other chronic conditions and twice as high among those with one other chronic condition than before cancer diagnosis. It remained stable for those with three or more conditions.
- Polypharmacy status after cancer diagnosis differed significantly by type of cancer. Among people with lung and bronchus cancers, only 31.7% were not on polypharmacy, compared with 53.5% of those with female genital cancer who were not on polypharmacy.
- 10.7% and 21.3% of the study population were high users of ER services and hospitalizations, respectively, in the year after cancer diagnosis.
- People with hyper-polypharmacy versus minor polypharmacy were 41% and 23% more likely to be high users of ER services and hospitalizations, respectively.
- Male sex, increasing levels of multimorbidity and cancer stages, and higher numbers of chemotherapy drugs were positively associated with both high use of ER services and hospitalizations. Cancers related to the digestive system, prostate and urinary system also were positively associated with high use.
As the prevalence of multimorbidity is increasing across age groups, additional studies of polypharmacy and its appropriateness are needed, wrote the authors, who declined to comment for this article. “Involvement of a multidisciplinary team that includes the input of clinical pharmacists is needed to monitor and adjust medication lists to reduce or control polypharmacy, and thus ensure optimal outcomes in adults, both young and old, with cancer and multimorbidity,” they said.
The study was well done in that it looked at patient populations across ages and cancer types, said Benyam Muluneh, PharmD, BCOP, CPP, an assistant professor of pharmacotherapy and experimental therapeutics at the UNC Eshelman School of Pharmacy, in Chapel Hill, N.C.
“The fact that they looked at younger adults is good, because a lot of conversations on polypharmacy are in older adults,” Dr. Muluneh told Pharmacy Practice News. “Cancer rates are increasing in the young adult population, so I think there’s a need to better characterize polypharmacy and other factors influencing care for young adults.”
People in their 20s, 30s and 40s are likely to be working and caring for young children or older parents, he added, and are therefore at higher risk for nonadherence to therapies. Therefore, pharmacists need to proactively check in with patients and perform medication reconciliation to ensure they are on optimal treatments, according to Dr. Muluneh. “There could be a better campaign to ensure that we’re talking about preventative care and medication-related adverse events with them with the same focus that we do with older adults,” he said.
Dr. Muluneh also said as some patients shop around for the best cost for orally administered chemotherapies, they are likely to patronize more than one pharmacy: “It’s really important to take time to get a medication history” and check for drug–drug interactions.
The sources reported no relevant financial disclosures.
{RELATED-HORIZONTAL}